In the evolving landscape of healthcare, several predictions we have for the coming year signal a paradigm shift in the industry. The commitment to prioritize patient outcomes, coordination, and preventive measures with the adoption of cutting-edge health technologies will remove historical barriers. This creates a more technologically advanced and patient-focused healthcare ecosystem. Please read below for our 2024 Healthcare Predictions:
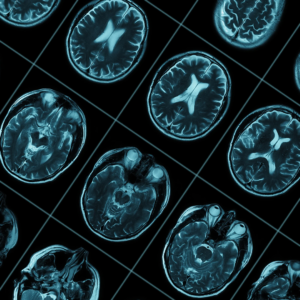
AI Revolution
This transformative shift involves leveraging artificial intelligence (AI) and cutting-edge health technologies to overcome barriers that have historically hindered access to quality care and envisions a significant transformation in the healthcare landscape driven by the widespread adoption and integration of AI. Here’s an exploration of the key components of this prediction:
- Transformative Shift: This suggests a fundamental and far-reaching change in the way healthcare is approached and delivered. This shift implies a departure from traditional models of care towards a more advanced and technologically driven paradigm.
- Leveraging AI: The prediction underscores the central role of artificial intelligence in driving this revolution. AI encompasses machine learning, deep learning, natural language processing, and other advanced technologies that enable computers to analyze data, learn from it, and make intelligent decisions. In healthcare, AI can be applied across various domains, including diagnostics, treatment planning, personalized medicine, and administrative tasks.
- Cutting-Edge Health Technologies: Beyond AI, the prediction references cutting-edge health technologies. This could include innovations such as wearable devices, remote monitoring solutions, telemedicine platforms, and other advancements that contribute to a more technologically sophisticated healthcare ecosystem.
- Overcoming Barriers: The focus on overcoming barriers indicates that the AI revolution is expected to address long-standing challenges in healthcare. These barriers could include issues related to accessibility, affordability, efficiency, and the ability to provide high-quality care to a broader population. Historical limitations in accessing quality healthcare are being targeted for improvement. AI is seen as a solution to enhance access to quality care, potentially by streamlining processes, improving diagnostic accuracy, enabling remote healthcare delivery, and making healthcare more patient-centric.
The “AI Revolution” anticipates a transformative era in healthcare where AI and cutting-edge technologies play a pivotal role in overcoming historical barriers to quality care. This suggests a future where advanced technological solutions contribute to a more efficient, accessible, and patient-focused healthcare system.
Consumerism in Healthcare
With higher out-of-pocket costs, consumerism is going to continue to expand. We will see companies like Headspace and Calm continue to grow with their Direct-to-Consumer (DtC) approach and 24/7 care. While retailers like Walmart and Amazon provide a clinical one-stop shop for screening, prevention, and intervention with an all-encompassing array of services. With the increasing costs and inflation within the medical industry, this has created the perfect storm to drive a rise in consumer-driven healthcare behavior. Here’s a breakdown of the key components of this prediction:
- Medical Inflation and Rising Costs: This part of the prediction anticipates a continued increase in healthcare costs, including expenses associated with medical services, treatments, and possibly insurance premiums. Medical inflation often outpaces general economic inflation, putting pressure on individuals to bear a larger share of their healthcare expenses.
- Higher Out-of-Pocket Costs: With the expectation of higher healthcare costs, individuals are likely to face increased out-of-pocket expenses, such as deductibles, copayments, and coinsurance. This shift places a greater financial burden on patients and prompts them to become more conscious consumers of healthcare services.
- Consumerism in Healthcare: The prediction suggests that as out-of-pocket costs rise, individuals will take a more active role in managing their healthcare choices. This consumer-driven approach involves patients making informed decisions about their healthcare options, seeking value for money, and being more selective in their healthcare-related purchases.
- DtC Approach: Companies like Headspace and Calm, known for providing mental health and wellness services, are expected to capitalize on the trend of consumerism in healthcare. Their direct-to-consumer approach means they engage with and provide services directly to the end-user without intermediaries. This could involve offering digital health solutions, virtual consultations, or other services that cater to consumers’ growing interest in taking control of their well-being.
- 24/7 Care: The mention of “24/7 care” suggests that there is an expectation for healthcare services to be available around the clock. This could involve continuous access to virtual health platforms, telemedicine services, or other forms of on-demand healthcare that align with the idea of consumers wanting convenient and timely access to medical care.
The economic pressures of medical inflation and rising costs drive individuals to become more actively involved in their healthcare decisions and demand convenience. Companies that offer DtC healthcare services, especially those addressing mental health and well-being, are anticipated to thrive in this environment by providing accessible, consumer-friendly solutions.
Continued Transition Towards Value-Based Care:
We anticipate seeing an ongoing shift in the healthcare industry towards a model that emphasizes the value delivered to patients rather than the traditional fee-for-service approach as we continue to see the following key elements expanded:
- Outcome Measurement: Instead of focusing solely on the quantity of services provided, value-based care measures the effectiveness of healthcare interventions by assessing patient outcomes, satisfaction, and overall health improvements.
- Care Coordination: Value-based care encourages better coordination among healthcare providers to ensure that patients receive comprehensive and well-coordinated care across different specialties and settings.
- Preventive Care: There is an increased emphasis on preventive measures to avoid the development of chronic conditions and to promote overall health and wellness.
- Payment Models: Reimbursement models are often tied to outcomes and patient satisfaction, incentivizing healthcare providers to deliver efficient and effective care. This can include payment structures such as bundled payments and shared savings arrangements.
- Health Information Technology: The use of technology, such as electronic health records (EHRs), data analytics, and telemedicine, plays a crucial role in supporting the transition to value-based care by facilitating better communication, data sharing, and coordination among healthcare providers.
- Patient-Centered Care: Value-based care places a strong emphasis on patient engagement and involvement in healthcare decision-making. It aims to tailor healthcare services to meet individual patient needs.
The transition towards value-based care is not a one-time event but rather an ongoing process that is continuing to gain traction and results. This indicates a sustained commitment to redefining and improving the healthcare delivery model for the benefit of both patients and the healthcare system as a whole.
Payors Addressing Health Equity
We believe we will see a more proactive approach by health plans (payors) in tackling health disparities and social determinants of health. Here’s a breakdown of the key elements of this prediction:
- Incorporating Unconventional Benefits: Health plans are going beyond traditional healthcare coverage by incorporating unconventional benefits. This indicates a recognition that factors outside the scope of medical care, known as social determinants of health, significantly impact an individual’s well-being.
- Comprehensive Approach to Social Determinants: Beyond addressing food insecurity, they may also offer services like transportation assistance for attending medical appointments and accessing fitness facilities, recognizing that these factors can impact health outcomes.
- Utilizing Quantitative and Qualitative Research Methods: Health plans are expected to employ a combination of quantitative and qualitative research methods. This implies a data-driven approach to understanding the needs and challenges faced by their members. Quantitative research involves analyzing numerical data, while qualitative research involves gathering insights from open-ended responses and narratives.
- Fostering Member Loyalty: In addition to improving health outcomes, health plans will expand on the impact of these initiatives on member loyalty. By addressing social determinants of health and providing unconventional benefits, health plans aim to create a positive impact on members’ lives and, in turn, build loyalty and satisfaction.
The shift in the role of health plans towards a more holistic and proactive approach, addressing social determinants of health and employing research-backed strategies to enhance health outcomes and member loyalty has begun and we are very excited to see this change in the healthcare evolution.
Looking Ahead to 2024
We hope you enjoyed our predictions and cannot wait to see what 2024 brings to the industry. Together, these predictions paint a picture of a healthcare future characterized by value-driven models, technological innovation, consumer-driven approaches, and a commitment to addressing social determinants for improved equity and overall well-being.